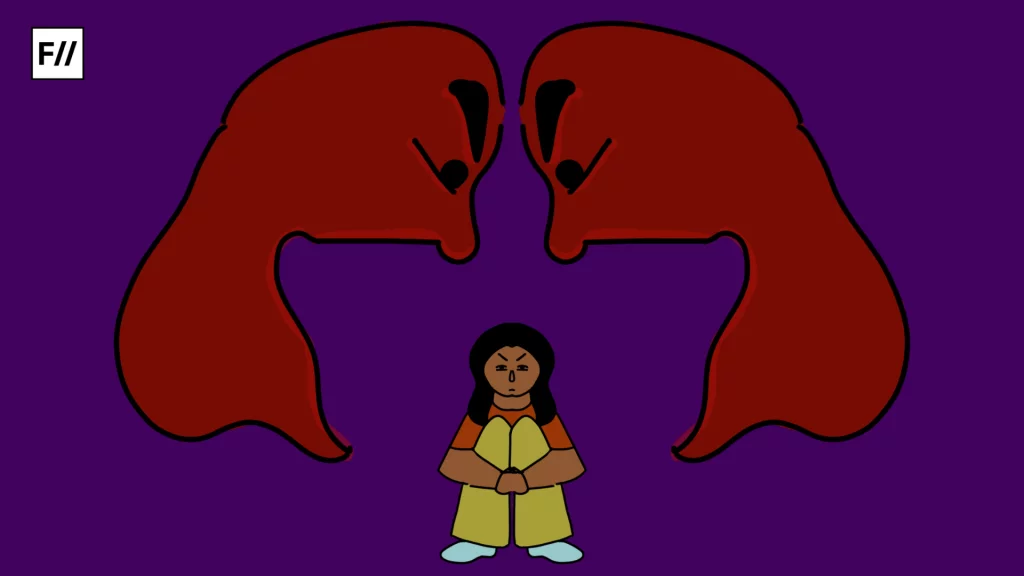
On a sweltering afternoon in May 2025, India’s Supreme Court posed a question that cut through decades of stigma: “Are we going to brand all transgender individuals as risky and stigmatise them?” The bench was hearing a petition challenging India’s blood donation rules, which permanently bar transgender people, men who have sex with men (MSM), and sex workers from donating blood. The judges’ concern was simple yet profound: why should an entire identity group be deemed unsafe when medical science has advanced so far that every unit of blood is rigorously screened for infection?
The case, filed by Santa Khurai, a transgender activist from Manipur, has put the spotlight on an uncomfortable truth: even as India celebrates legal victories like the decriminalisation of homosexuality in 2018 and the recognition of transgender rights in 2014, its healthcare system remains tethered to discriminatory assumptions. At stake is not just the dignity of marginalised communities but also the nation’s blood supply, already facing an annual shortfall of up to two million units.
Blood donation policy written in fear
India’s blood donor policy is laid out in the 2017 “Guidelines on Blood Donor Selection and Referral,” drafted by the National Blood Transfusion Council (NBTC) and the National AIDS Control Organisation (NACO). Clauses 12 and 51 of these guidelines label transgender people, gay and bisexual men, female sex workers, and intravenous drug users as “high-risk” groups. The label carries permanent consequences: members of these communities are barred for life from donating blood, regardless of their actual sexual practices, monogamy, or medical test results.

The government defends these rules as precautionary. Officials argue that India’s HIV prevalence among MSM, estimated at 2.7%, compared with 0.2% in the general population, is reason enough for blanket bans. “We cannot take chances when it comes to transfusion safety,” a senior health ministry official told the court in an affidavit earlier this year. However, critics argue that this logic is deeply flawed. Instead of assessing risk based on behaviours, such as unprotected sex or multiple partners, the policy assumes that entire communities are inherently unsafe.
For many queer men in India, the blood donation ban is more than a policy—it is a deeply personal reminder of exclusion. Sameer, a 28-year-old gay man from Delhi, recalls being turned away at a corporate blood donation drive.
‘I remember filling out the form and hesitating when I saw the question about sexual history. I decided to be honest, and the staff quietly told me I couldn’t donate. It felt humiliating.
This approach, activists argue, entrenches social stigma. ‘By barring us from donating, the state brands us as dirty,’ Khurai said in a statement after the hearing. ‘We want to save lives, too. But our blood is considered tainted before it is even tested.’
Voices from those affected
For many queer men in India, the blood donation ban is more than a policy—it is a deeply personal reminder of exclusion. Sameer, a 28-year-old gay man from Delhi, recalls being turned away at a corporate blood donation drive. ‘I remember filling out the form and hesitating when I saw the question about sexual history. I decided to be honest, and the staff quietly told me I couldn’t donate. It felt humiliating. I walked out pretending I was unwell, just so my colleagues wouldn’t ask questions. It’s like the system is telling me I’m unsafe, even though I get tested regularly.’
For others, the policy creates impossible dilemmas in moments of crisis. Arjun, 32, from Bengaluru, says he once considered lying on the donor form when a close friend needed blood urgently. ‘I’m in a monogamous relationship, I test every few months, and I’m healthier than many straight guys I know. Still, I knew I’d be rejected. I actually thought about lying just to help, but I didn’t want to get anyone in trouble. That’s when it hit me—this rule isn’t just discriminatory, it can actually cost lives.’ These experiences highlight how blanket bans not only alienate willing donors but may also worsen India’s blood shortages, which already stand at nearly one to two million units annually.
For transgender people, the ban reinforces a lifetime of stigma. Meera, a 27-year-old trans woman from Jammu, says such policies cut deep: ‘Sometimes it feels like no matter what we do, we’re seen as a threat. We already fight every day just to be accepted in our families, in our jobs, on the streets. And then rules like this come along, telling people that we’re not normal, that our blood isn’t clean. It breaks your heart. We’re not asking for special treatment—just the chance to be seen as human.’
A legal reckoning and the human cost of stigma
The Supreme Court’s scrutiny of India’s blood donation guidelines comes at a time when the nation’s jurisprudence on LGBTQ+ and transgender rights is expanding. In 2014, the landmark NALSA v. Union of India judgment recognized the right of transgender persons to self-identify their gender. Four years later, the Court struck down Section 377 of the Indian Penal Code in Navtej Singh Johar v. Union of India, decriminalizing same-sex relationships.

Yet despite these advances, India’s 2017 blood donor guidelines continue to classify transgender persons, men who have sex with men (MSM), and sex workers as “high-risk” donors, effectively banning them. Khurai argues that this violates Articles 14 and 15 of the Constitution, which guarantee equality and prohibit discrimination, and Article 21, which safeguards dignity and life. The petition also cites the Transgender Persons (Protection of Rights) Act, 2019, which explicitly prohibits discrimination in healthcare. “These guidelines stigmatize us at a structural level,” Khurai told reporters. “They send the message that we are unfit citizens, even as we fight for the right to live.”
Arjun, 32, from Bengaluru, says he once considered lying on the donor form when a close friend needed blood urgently. ‘I’m in a monogamous relationship, I test every few months, and I’m healthier than many straight guys I know. Still, I knew I’d be rejected.
The bench, led by Justices S. Ravindra Bhat and Aravind Kumar, has pressed the Health Ministry to seek expert consultation. While the government insists the ban is a necessary precaution, the court’s skepticism signals growing recognition that safety and inclusion are not mutually exclusive. For LGBTQ+ Indians, this is not merely a medical debate but a deeply symbolic one. Many recall being turned away from blood drives at schools or offices, forced to disclose their sexuality or gender identity in humiliating ways. The stigma carries heavy consequences. According to a 2017 NHRC study, 96% of transgender persons are denied jobs, and 60% lack access to healthcare.
Public health experts say the solution is clear: adopt a behaviour-based screening model that asks all donors the same questions about sexual activity, drug use, or travel history, followed by universal testing. India already has over 3,000 licensed blood banks, and many tertiary hospitals use Nucleic Acid Testing (NAT) to detect infections.
India’s blood shortage crisis
India’s blood shortage is not just a number—it is a matter of life and death. According to government data, the country requires around 14.6 million units of blood annually, yet supply often falls short by one to two million units. This deficit can delay life-saving surgeries, complicate childbirth, and undermine cancer treatment. During dengue and malaria outbreaks, demand spikes even further, straining blood banks already operating on the brink.

Ironically, communities excluded from donating blood often know firsthand what shortages mean. Many transgender people, who face barriers to employment and healthcare access, rely on blood transfusions during surgeries and medical emergencies.
The world has changed
When India’s guidelines were written, blood transfusion safety depended heavily on screening donors through questionnaires, as laboratory tests were limited. Today, that has changed dramatically. Every unit of blood in India is tested for five transfusion-transmissible infections (TTIs): HIV, Hepatitis B, Hepatitis C, syphilis, and malaria. The use of fourth-generation ELISA tests and Nucleic Acid Testing (NAT) has reduced the “window period”—the time between infection and detectability—to just a few days for HIV and other viruses.
For transgender people, queer men, and sex workers, this blood donation ban is not just a medical policy—it is a public declaration that their lives and their humanity are less valuable.
Science has advanced, testing systems have improved, and other nations have shown that behaviour-based screening can keep blood supplies safe without dehumanizing entire communities. Yet India’s policy still clings to outdated fears, turning away willing donors whose only “risk” is who they are.
Other countries have already moved away from blanket bans. The UK was first in 2021, replacing its three-month abstinence rule for gay and bisexual men with a behaviour-based system: all donors, regardless of gender or orientation, answer the same questions about sexual activity in the past three months. Canada followed in 2022, after years of research and pilot studies, implementing gender-neutral screening that focuses only on risk behaviours—not identity.
In 2023, the United States FDA lifted its long-standing restrictions, allowing gay and bisexual men in monogamous relationships to donate. The new U.S. rules introduced a universal questionnaire for all donors, relying on advanced nucleic acid testing to ensure safety. Officials emphasized a simple principle: “It’s not who you are, but what you do that matters.” Together, these countries show that inclusivity and safety can coexist, providing a roadmap for India, where an annual shortfall of nearly 1.9 million blood units (NACO) makes every willing donor critical.
India at a crossroads
India stands at a crossroads. Science has advanced, testing systems have improved, and other nations have shown that behaviour-based screening can keep blood supplies safe without dehumanizing entire communities. Yet India’s policy still clings to outdated fears, turning away willing donors whose only “risk” is who they are. For transgender people, queer men, and sex workers, this is not just a medical policy—it is a public declaration that their lives and their humanity are less valuable. Every unit of blood is a chance to save a life, and every rejection is a missed opportunity. In a country grappling with persistent shortages, the exclusion of entire communities is not only unjust but dangerous.
To deny them the right to give is to deepen a cycle of stigma and scarcity; to welcome them as equals would be to affirm that their blood, like their dignity, is not up for debate.The Supreme Court’s challenge is an invitation to reimagine public health through a lens of both science and justice. India can lead by example—choosing policies that protect safety without perpetuating shame, and building a future where compassion, not prejudice, flows through the nation’s veins.
About the author(s)
Masrat Nabi is a journalist whose work focuses on politics, gender, culture, and social issues in India.