It has been well-documented that individuals in low- and middle-income countries bear disproportionate health consequences of cancer. Specifically, 70% of deaths in these countries caused by breast cancer occur in people younger than 70 years of age. Under such circumstances, the situation in India compared to that of high-income countries leaves much to be desired, with its ‘low 5-year survival rate‘ for breast cancer and median age of diagnosis under 47.
Recently published studies in this field have further highlighted the income disparities within India that make it harder for individuals and families to access health care.
Recently published studies in this field have further highlighted the income disparities within India that make it harder for individuals and families to access health care. Even if healthcare is available, it comes at a huge cost. The study in question was conducted by researchers Mohanty et. al from the International Institute of Population Science (IIPS) and was published in The International Journal for Equity and Health on July 23rd. The health expenditure of 500 breast cancer patients in Tata Memorial Centre, Mumbai, India was followed over three years: from June 2019 to March 2022.
What makes this study significant, is that it is the first study to attempt to estimate the ‘exact extent of catastrophic health spending‘. The World Bank describes catastrophic health spending as expenditures on health that exceed a certain percentage of a household’s income. This percentage can be set at different levels, anywhere from 10%-40%. For example, if the threshold is determined at 10%, then a household’s spending is considered catastrophic if it spends more than 10% of its income on healthcare.

According to its findings, the level of catastrophic health spending in India is around 85%, and those who depend on agriculture as their primary source of income are the worst affected. 3/4th of households with cancer patients had to go to great lengths in order to cover cancer treatment costs. While some borrowed money, others sold their assets: ‘A mere 5.8% of the patients used income as one of the sources for covering treatment cost, 48.6% used savings, 66.6% had resorted to loans & borrowings and 72.4% had either sold assets or borrowed to finance the cost of treatment.‘
While health insurance certainly helps, it only reduces the financial burden caused by expenditure on health by 13%. This indicates that last-minute fixes are not as helpful as one is led to believe. What is needed, then, is to identify the circumstances that push individuals at risk of breast cancer into such financially and emotionally insecure situations in the first place, and what can be done to prevent these outcomes.
Breast cancer in India
Thus, in order to understand the importance of these findings and the dire consequences faced by individuals, it is necessary to first contextualise them against the number of breast cancer cases in India. According to the same report, India has the third highest number of cases worldwide, making up 8.4% of 2.3 million cases.
What makes the situation worse is that this percentage would have been higher if screening for breast cancer in India were more popular.
What makes the situation worse is that this percentage would have been higher if screening for breast cancer in India were more popular. Currently, only 0.9% of women undergo screening for the same. Another study from December 2022 by Sen et al. showed that the proportion of breast cancer screening per 100,000 women in India was only 877. The percentage is even lower for uneducated women in rural India. In this regard, India is worse off than many other developing countries.

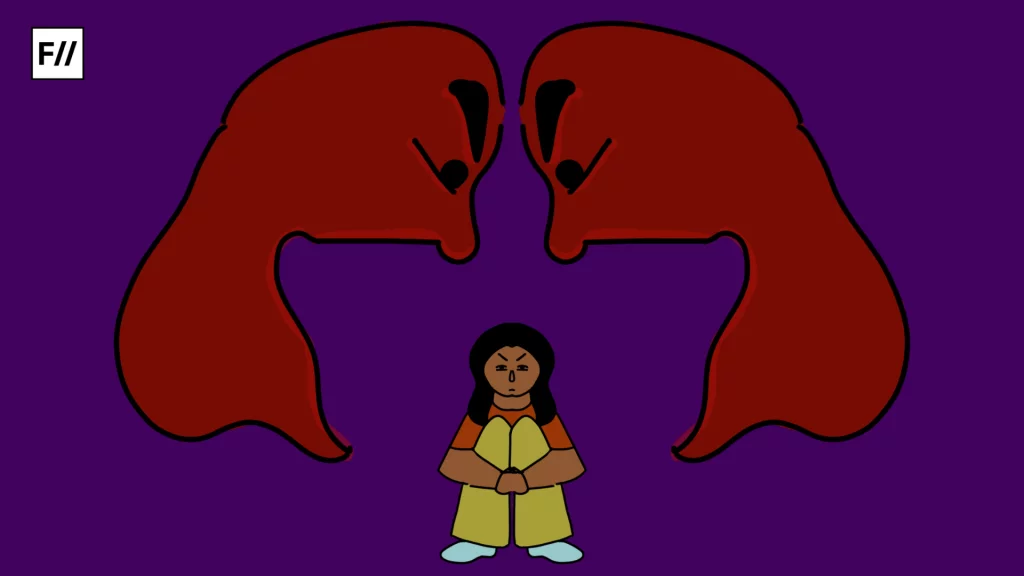
One evident reason behind these low screening rates is the secondary socio-economic status women occupy in their households and the country at large; the heavy financial burden of health costs only worsens their situation. Tripathi et al. conducted a study to further understand the context-specific barriers rural women face that prevent early detection of cancer, other than the lack of medical institutions. They surveyed 281 women and gauged general knowledge levels about the curability of several types of cancers (breast, oral, cervical), their symptoms and screening procedures.
Most women, i.e. 84.93% stated that they did not know how to perform a Breast Self-Examination or a BSE. 15.07% did not have enough time to conduct one, and 0.46% reported having no privacy to do so. These are significant insights into the causes and barriers that women face. If addressed adequately, they can prove to bolster the effectiveness of existing medical institutions (and when established in the areas that do not have them). Low awareness about risk factors for breast cancer, about 30%, stops early detection which in turn makes cure difficult: as the age of diagnosis increases, the survival rate for breast cancer patients decreases. Additionally, Mohanty et al. state that late-stage detection prolongs treatment periods further increasing health expenditure.
What can improve the situation?
The reality is grim, and urgent efforts are needed to change the lives of those worse affected by breast cancer. Resilient change can only be brought about by improved medical infrastructure, especially in rural India. However, until then, raising awareness about Breast Self-Examination should be a starting point. After all, according to the National Breast Cancer Foundation and the Distinguished Service Professor of Breast Cancer at Johns Hopkins University, Lillie D. Shockney, 40% of diagnosed breast cancers are first discovered in this way.

Thus, by improving early-detection levels, the expenditure on health can be curbed to a certain extent. For a thorough self-examination, the following three steps must be followed without fail:
- Perform a self-examination in the shower: Every month, the breast and armpit area should be checked. Using the pads of three middle fingers and applying medium but firm pressure, new lumps, if any, must be identified and made note of.
- Perform one while standing in front of a mirror: Visual inspection can also help identify any irregularities such as swelling or sudden changes in the shape of the breasts or the area around the nipples. Another way of carrying out this inspection is by flexing the chest muscles. One should be on the lookout for similar changes as the ones noted above.
- Perform one while lying down in bed: A pillow should be placed under one’s right shoulder and the right arm should be behind the head. Then, the self-examination is to be performed in the same way as it is to be done in the shower. Any discharge must also be made note of.
About the author(s)
Aaliya Bukhary (she/her) is student of Economics student based in Mumbai. She is passionate about merging data analysis with her love for writing, and aspires to empower through information. Aaliya also has a fondness for cats and enjoys listening to Mitski!