“Its so difficult to describe depression to someone who’s never been there, because its not sadness.” – J.K. Rowling.
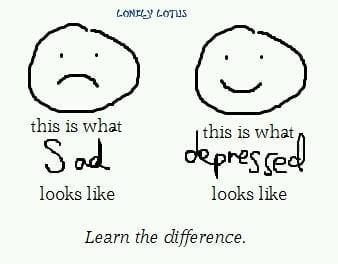
We often use the word ‘depressed’ to refer to something which makes us sad. Words like ‘depressing’, ‘depressed’, or ‘depression’ itself are often used to express sadness – if we introspect a bit on this we will realise that this is fairly common. This article seeks to go into the difference between being ‘depressed’ and being ‘sad’ and how the use of the two terms interchangeably actually makes a difference and reflects upon the general understanding of mental illness.
Psychology has recognised that distinguishing between sadness and depression is of clinical importance for two broad reasons – it serves as a starting point for moving into the realm of illness; and is also consistent with common sense. It is in the larger public interest that we must be able to define mental disorders with some accuracy just as it is necessary that we determine the pathological potential of a virus.
People are often unable to tell the two states apart and hence end up being confused about their own mental state. Therefore for a basic self-diagnosis it is important to be able to tell the difference between sadness and depression.
The difference between sadness and depression has broadly got to do with symptoms and their severity. While there is often an overlap of symptoms, the two remain distinct. Sadness is considered to be one of the many human emotions that we all experience throughout our lives, just like happiness, fear or anger. Depression, on the other hand, is a condition in itself with a complex manifestation of emotions, thoughts (cognition) and physical symptoms. Therefore it is far more than just a feeling or having a bad hair day. Sadness is believed to be triggered by an event and a response proportionate to it; whereas depression need not necessarily have a definite traceable cause and is disproportionate in terms of response and its duration.
it is important to be able to tell the difference between sadness and depression.
Diagnostic and Statistical Manual of Mental Disorders (DSM-V) lays down the symptoms for depression, some of which are – insomnia or over-sleeping, loss of appetite, low concentration level, negative thoughts, low self-esteem and physical conditions like headaches and fatigue. Specialists look for these symptoms before diagnosing clinical depression. One very significant feature of depression is loss of interest or pleasure in activities. A complete loss of interest has often been associated with someone suffering from depression. Therefore this is one distinctive symptom that one can look out for in determining someone else’s mental state. The Manual requires the presence of five or more such symptoms for more than two weeks.
At the same time it is argued that it is not always possible to diagnose clinical depression with precision. Therefore it is not that someone is denied any help because their symptoms do not meet the criterion laid down in DSM-V – it is that the kind of the treatment/help they receive varies.
This is where the understanding the difference in the kinds of psychological treatment or help becomes very important. There are three kinds of specialists – counsellor, psychologist/therapist and psychiatrist.
It is important to not just get the illness right but also the treatment of it.
A counsellor is trained in Psychology, generally up to Master’s level. They are licensed professionals but the scope of their practice is limited. They deal with a varied range of problems and help the patient to reach a preferable solution; but they cannot administer psychological assessments or medicines. A therapist, however, is licensed to administer proper psychological treatment using various kinds of psychological therapies. Therapy is a continuous treatment and therapists are not authorized to prescribe drugs. A psychiatrist on the other hand, is a doctor trained to diagnose and treat mental illness by prescribing medicines etc.
Also Read: Do I Need A Therapist? These Three Things Will Help You Decide
It is important to not just get the illness right but also the treatment of it. Depending upon the severity of someone’s state, they can seek help from these different kinds of professionals. A counsellor may refer to a therapist if she is convinced that psychological therapy is required and counselling sessions are being ineffective.
Conflating sadness and depression makes us either over-value or under-value someone else’s problems. This has greater repercussions when we think that a person suffering from clinical depression is just sad or down. This makes us say things like, “Snap out of it!”, “Everyone has those days” or “Everything is fine, it is all in your mind”. The same lack of understanding makes us soon lose empathy and patience with the mentally ill and ignore them. None of these responses are conducive to alleviating the mental agony of someone suffering from clinical depression; they only serve to only aggravate it. Hence this confusion and conflation leads to isolation of the one who is mentally ill and reduces their chances of getting help. When we use the two terms interchangeably we equalize concepts which are not equals – they are different in their manifestations and severity.
Also Read: How Your Tough Love Hurts People With Depression And What To Do Instead
Conflating sadness and depression makes us either over-value or under-value someone’s problems.
Depression is a mental illness and goes beyond sadness. Conceptual clarity is a crucial step to increasing awareness about mental health and mental disorders in the society. If we want to change our attitude towards mental illness then it is only plain that we should be able to appreciate the difference between sadness and depression.
About the author(s)
Madhulka is a third-year law student. Her areas of interest include laws relating to women, human rights and history. She likes to watch Marvel movies and period cinema in her free time.