As open as I am about talking about my sexual organs, visiting my gynaecologist has always left me feeling unsettled. One time, after what felt like an eternity of her examining me, she asked me if I was going to get a Pap smear. In two minutes, she explained to a very clueless and shocked nineteen year old that I (and probably all of my female friends) am at a risk of cervical cancer and since it’s too late to get vaccinated now, we should start getting tested soon. The walk back home had me upset – why hadn’t I known about this? Did anyone else know about vaccinations? No matter where I went, the answer was a resounding “no”. Even my mother didn’t know what Pap smears were for.
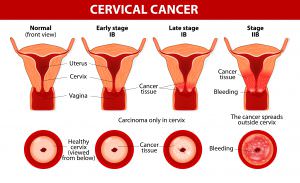
Cervical cancer is caused in the cervix i.e. the mouth of the uterus in women. The cervix is the narrow part of the uterus. The cancer occurs when abnormal cells on the cervix continue to grow. It can be fatal and 510,000 women die globally each year as a result of cervical cancer.
The major cause of cervical cancer is by the contraction of the Human Papilloma Virus (HPV) and while there are many serotypes of the virus, the types HPV-16 and 18 are the ones that cause cervical cancer. Cervical cancer can start affecting women around the age of 30-34. According to World Health Organisation (WHO), administration of cervical cancer vaccines to everyone would end up saving thousands of lives and improve the health of girls and women all over the world.
Personally, I wasn’t aware of the existence of vaccinations to prevent cervical cancer until last year. Cervical cancer vaccines entered India in 2006. The vaccines essentially prevent the body from contracting and spreading HPV, which is the leading cause of cervical cancer.
510,000 women die globally each year DUE TO cervical cancer.
Types of Cervical Cancer
The two main types of cervical cancer vaccines in India are Gardasil™ and Cervarix™, which prevent the body from contraction of HPV types 16 and 18. Gardasil™ needs to be administered in three doses at 0, 2 and 6 months, and Cervarix™ needs to be administered in three doses at 0, 1, and 6 months. While Gardasil™ can protect someone against cervical cancer and genital warts, Cervarix™ only provides protection against cervical cancer.

Clinical trials of both vaccines reveal results that were a huge success. About 16,000-18,000 women aged between 16-26 remained uninfected by HPV after being vaccinated with Gardasil and Cervarix, who showed 90-100% efficacy against the serotypes of HPV which cause cervical cancer. The follow up time for these vaccines is around 15 months to two years, and studies showed no evidence of harm to immunity and health.
The number one cancer that affects Indian women is cervical cancer.
While HPV is not a cause for cervical cancer alone, its co-factors such as use of hormonal contraceptives, poor hygiene, a diet lacking in antioxidants, tobacco consumption and sexually transmitted infections often help in progression of HPV into the cancer, and so the administration of the vaccine(s) becomes important so that an absence of HPV prevents the cancer altogether.
HPV Vaccine

It is recommended that cervical cancer vaccines be taken between the ages of 9-12 years and catch-up vaccines must be taken within 26 years. The current costs of both types of vaccines are Rs. 2,700-3,000 for Gardasil and about Rs. 2000 for Cervarix. The vaccines are not available at state hospitals and government hospitals, and to get administered with the shots, a person has to visit a private hospital clinic.
The number one cancer that affects Indian women is cervical cancer. The 365 million Indian women who are above the age of 15 are at a high risk of developing HPV and subsequently are at the risk of developing cervical cancer. India currently accounts for approximately one-fourth of the world’s cases of cervical cancer. Recent statistics report about 64,000 deaths of Indian women caused by this type of cancer.
The fatality and commonness of cervical cancer is not the only reason why we need vaccination against it. Cervical cancer is known as a silent killer – women who have been or are sexually active are at higher risk of developing HPV, and at early stages, cervical cancer shows no visible symptoms. Only as the cancer grows does the person start experiencing symptoms such as cramping, urinary tract infections, abnormal vaginal discharges and irregular menstruation. The problem is that these kind of symptoms do not directly point to cervical cancer at all times as they are also indicative of other problems like sexually transmitted diseases, urinary tract infections and simple hormonal imbalance leading to shift of menstrual cycles.
It is recommended that vaccines be taken between the ages of 9-12 years and catch-up vaccines be taken within 26 years.
Prevention
To detect cervical cancer, the most effective procedure is known as a Pap smear, which screens for the presence of cancerous or precancerous cells on the cervix. Pap smear costs start at Rs. 1,000 per screening. For the women in India coming from lower income backgrounds and rural areas, an earning of average Rs. 120 per day (which is 56% of what their male counterparts earn), from which they have to cater to the financial needs of their families, pap smears are too expensive a cost to bear. Many women in India are unable to afford Pap smear tests and are also subsequently unable to afford treatment of cervical cancer, through radiotherapy, chemotherapy or surgery, the costs of which are estimated from over Rs. 2,00,000.
The existing discussion around the kinds of cancers that affect women, cervical cancer is not given the requisite attention despite its commonality. Lack of awareness about the cervix and cervical cancer acts as a major barrier to women seeking treatment for the same. A study conducted among female students in Kolkata, which showed that only 20% of the subjects knew about cervical cancer, is indicative of the awareness of people in India. This points to how much worse the condition would be amongst women who cannot access education and hence are not aware of sexual health and their bodies, let alone be aware of cervical cancer. The taboo around women’s bodies and vaginal health also prevents women from accessing gynaecological help, and women from lower income backgrounds are unable to seek even basic gynaecological care. There is a also a high shortage of gynaecologists all over India, significantly adding to the problem.
In this scenario, prevention from cervical cancer is undeniably a better option than treatment. Cervical cancer vaccines are not only a cheaper alternative but also a better alternative as it eliminates the development of HPV-16 and 18, which makes it impossible for the cancer to develop against this immunity. It is estimated that the cost of cervical cancer vaccinations if made a mandatory vaccine would come out to Rs. 900 per vaccine, and this definitely counts for a more affordable avenue than treatments and tests.
Discussion around the provision of state-funded cervical cancer vaccines often leads to the criticism that the cost is too expensive, but some vaccinations provided by the government under the immunisation programme cost approximately Rs. 1,000 to vaccinate everyone, and so evidently the medical benefits of cervical cancer vaccines outweigh the costs.
The government advocates for cost-effective screening tests, but it’s unreasonable to invest in this sort of roulette with the lives of women; cancer-positive results of the screenings end up creating the further requirement for expensive treatments, which can differ according to the stage the cancer is at – the worse the cancer, the more expensive the treatment. Furthermore, conducting large scale screenings which must happen routinely in order to detect cancer early proves to be extremely difficult to achieve.
Cervical cancer inevitably is a pubic health concern. Genital HPV difficult to prevent without lifetime abstinence, and there is no coherent evidence which shows how protection (like condoms) can help in preventing HPV. It then becomes incumbent on the welfare state to pay attention to the many women who are exposed to the risk of cervical cancer in India and thus prioritise investment towards the research and prevention, and cervical cancer vaccines have proven to be extremely effective. By providing vaccines to all girls in India, it ensures that the cancer is prevented in all Indian women, just as the government-provided vaccinations against polio and smallpox prevent the disease in the population.
Many women cannot access private hospitals where vaccination is available, and seeking protection against cervical cancer should not be a matter of accessibility dependent on socio-economic standards of living; this protection should be available to all women regardless of circumstances. Investment and attention to cancer vaccines also act as a progressive change in women’s health and improves the scope of sex education and will increase awareness of sexual health.
About the author(s)
Tanya is a law student who hopes to make the world a better place for people of all genders, sexes, and sexualities. She also has an undying love for theatre, music, and biryani.




Good article.Articles like these are really required and are the need of the hour to spread awareness about it.Cervical Cancer is spreading like a menace and young girls need to be cautions about it especially those who are sexually active.However the good news is that it can be easily detected and cured.
Cancer need to address effectively.
Great information. I was looking for the same
thanks for sharing Valuable information