Editor’s Note: This month, that is November 2020, FII’s #MoodOfTheMonth is Sexual And Reproductive Health, where we invite various articles to highlight how health outcomes are determined with respect to a person’s social, political, economic and cultural contexts of their gender and sexuality, and how these identities shape their life experiences vis-a-vis SRHR in India. If you’d like to share your article, email us at pragya@feminisminindia.com.
The first time I heard the term ‘endometriosis’ was at thirty-three. I had painful periods from as long as I can remember but it took me that long to get a diagnosis. I had been seeing my English GP for the last five years complaining of constant lower abdominal pain only to be told that it is possibly a Urinary Tract Infection. Laboratory results revealed that was not the case. After five years of suffering like this, I visited India to seek treatment. My gynecologist who had seen me from the time I was twenty-years-old thought something was amiss. She did not think it was normal that my periods were painful.

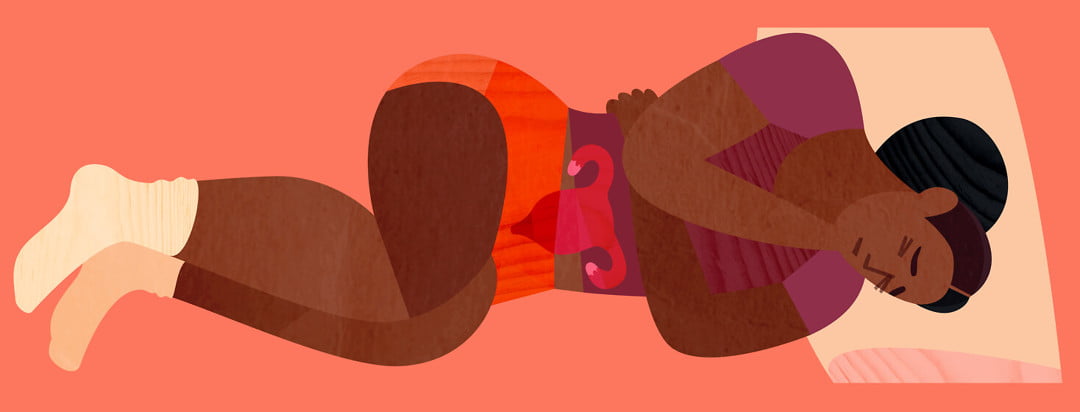
Image Source: British Journal of Family Medicine
I was prescribed a lapro-hysteroscopy, an intervention that required the surgeon to take a closer look at my uterus, cervix, fallopian tubes and ovaries by making small incisions on my abdomen (laparoscopic surgery) and also inflate the uterus to closely examine it. The procedure required general anesthesia and the doctor suspected it might take half an hour and a day’s stay at the hospital.
It took three and a half hours and three days of stay at the hospital. It turned out I had grade-3 endometriosis. Endometriosis is a condition in which “…the endometrium (the tissue that lines the inside of the uterus or womb) is present outside of the uterus. Endometriosis most commonly occurs in the lower abdomen or pelvis, but it can appear anywhere in the body” (UCLA Health). The severity of endometriosis is graded (1-4) depending on whether it is mild, moderate or severe, with the last two grades being considered the worst. It is not clear what causes endometriosis but the physiological reason is the backflow of menstrual blood and tissues into the body instead of being completely removed during monthly cycles.
To the doctor looking inside your body, endometriosis presents itself in the following manner – in a mild case (stage 1) there are several examples of endometrial tissues in the peritoneum, the abdominal cavity that contains all our organs except our kidneys and adrenal glands.
In the second stage, there are chocolate cysts (a cyst made of endometrial tissue and blood) that has proliferated the ovaries and has the tendency to spread to other organs (adhesions).
In the third stage, endometriosis has spread beyond the ovaries and can even be seen in the rectum and the bladder in some cases.
In the fourth, which is the most severe case, endometrial tissues can be found outside the pelvic and abdominal cavity in the heart, lungs and also the brain.
Stages three and four are the most complex to manage medically and also cause immense suffering to the individual; therefore early diagnosis is critical.
To the sufferer, endometriosis presents itself with some classic symptoms—lower abdominal pain, pain with menstrual periods, pain during sexual intercourse, and difficulty getting pregnant. Despite this, it took more than five years of suffering for me to get a diagnosis.
To the sufferer, endometriosis presents itself with some classic symptoms—lower abdominal pain, pain with menstrual periods, pain during sexual intercourse, and difficulty getting pregnant. Despite this, it took more than five years of suffering for me to get a diagnosis. Endometriosis had caused adhesions and scarring where the tissue had grown outside my womb that needed to be scraped off during surgery, my uterus was infected, one ovary had completely lost functioning and the fallopian tubes were damaged.
I remember a very kind surgeon holding my hand, as I lay in the frigid recovery room slowly regaining consciousness, trying to be as assuring as he could. I asked him to tell the truth and the damning verdict was delivered—my chances of getting pregnant even through In Vitro Fertilization (IVF) was very low. I could try it once to exhaust all possibilities, but donor eggs were the best possibility for me.
I was shocked, upset and very angry. How was it that despite repeatedly seeking assistance from my English GP, my condition had not been diagnosed? Why were my repeated complaints of pain not taken seriously? As a researcher working on reproductive, maternal and women’s health, I had access to greater information, yet I had not managed to convince my GP to do further investigations.

I subsequently discovered my experience was not unique. Research by the BBC in which over 13,500 women participated revealed that it takes an average of 7 years in the UK to diagnose endometriosis which affects 1 in every 10 women. Some women revealed that the pain was so debilitating that it made it impossible for them to sit up during their periods, others had become addicted to opiates to manage their pain, some like me had lost their ability to become pregnant naturally while many had suffered from pain during sex or while passing urine or stool since endometrial tissue can grow over bladder and the bowel.
Also read: Endometriosis: Journey Of Loving Myself, My Body A Little More
Endometriosis does not develop in the same way for all women. For some, the symptoms start when they begin their periods and for others it develops over their teenage years and their early twenties. The pain is often described by sufferers as having a knife being stabbed repeatedly in their lower abdomen. For a minority who have a very severe form, a complete hysterectomy where all the reproductive organs including ovaries, fallopian tubes and the uterus are removed is the only solution.
For others, a partial hysterectomy, where some of the reproductive organs are removed is advisable. For those who were lucky enough to not have such extensive damage, or when it is diagnosed early a hormonal IntraUterine Device (IUD) is used to balance hormones to mitigate against the growth of the endometrium outside the uterus.
If diagnosed early, there are multiple treatment options. However, early diagnosis requires women’s menstrual pain is taken seriously by physicians and family members, and not normalised, that there is greater sensitivity among physicians, that severe period pain requires further investigations, and that as women we are proactive about our endometrial health and aggressively advocate for ourselves. Medicine has a long history of undermining, misdiagnosing and underdiagnosing several conditions in women, including endometriosis.
If diagnosed early, there are multiple treatment options. However, early diagnosis requires women’s menstrual pain is taken seriously by physicians and family members, and not normalised, that there is greater sensitivity among physicians, that severe period pain requires further investigations, and that as women we are proactive about our endometrial health and aggressively advocate for ourselves.
The Endometriosis Foundation of India estimates that there are 25 million women in India who suffer from this condition. Very few have access to treatment options which can become very expensive the longer it takes to diagnose the problem. It’s only in recent years that we have begun to discuss menstruation openly with even our honourable Prime Minister mentioning sanitary pads in his Independence Day address! This is an opportunity for having more sustained and meaningful conversations, awareness campaigns and sensitisation practices around the whole range of issues that affect so many women’s reproductive and sexual health.
Also read: Zomato’s Period Leave Policy And The Feminist Dilemma Around It
Endometriosis is a painful condition that is debilitating for some women with long-term impacts on women’s reproductive, sexual and psychological health. For this reason alone, it deserves much greater attention than it receives at the moment. So, if you are a young woman gritting your teeth through painful periods or any of the other symptoms described here, thinking this is one of the many downsides of being born female, it’s time to visit a gynecologist. If they do not take your complaints seriously, push them and keep pushing until you have an answer.
Don’t suffer silently. Your body and mind will thank you in the long run.
About the author(s)
Sreeparna Chattopadhyay has a Ph.D. in Cultural Anthropology from Brown University with research interests in gender and its intersections with health, education family and the law. She is an independent researcher.



I’m really glad that FII is providing a platform to talk openly about experience with endometriosis. Kudos to the author for coming forward with her story in such an informative manner.