The Finance Minister of India, Nirmala Sitharaman, in the Interim Budget 2024-2025 speech, stated that the “government will encourage vaccination for girls in age group of 9 to 14 years for prevention of cervical cancer.”
According to recent data, cervical cancer is the 4th most common cancer among women worldwide and the rates of cervical cancer and mortality are highest in low and middle-income countries. In India, cervical cancer is considered the 2nd most prevalent cancer in the country.
Vaccination for cervical cancer prevention and barriers to HPV vaccination
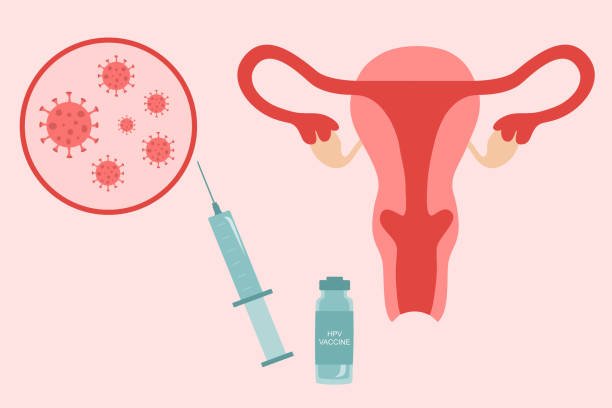
95 per cent of cervical cancers are caused when persistent infection of the cervix with human papillomavirus virus (HPV), a sexually transmitted infection (STI), is left untreated. Vaccinating individuals between 9 to 14 years has proven to be highly effective in preventing HPV infection, cancer of the cervix and other HPV-related cancers.
Yet, the World Health Organisation (WHO) found that as of 2020, the HPV vaccine was not part of India’s national vaccination program.
The Universal Immunisation Programme (UIP) in India is one of the largest public health programmes targeting close to 2.67 crore newborns and 2.9 crore pregnant women annually. Under UIP, immunisation is free of cost against 12 vaccine-preventable diseases. The HPV vaccine is currently not part of the National Immunisation Schedule. While the reason behind this is not clear, it is worth noting that a previous initiative to introduce the HPV vaccine as a public sector benefit in India was mired in legal controversy.
From 2009 to 2010, a cervical cancer vaccine demonstration project was conducted in India through a collaboration between PATH (an international NGO), Indian Council of Medical Research (ICMR) and the states of Gujarat and Andhra Pradesh. As per PATH, the project was envisaged as a ‘post-licensure observational study‘ to administer HPV vaccines to 24,000 tribal and marginalised girls in Gujarat and Andhra Pradesh.
A ‘post-licensure observational study‘ of a medical product is carried out to detect adverse events related to the product’s use, not identified before its licensing. The vaccines (‘Gardasil’ manufactured by Merck and ‘Cervarix’ by GSK Pharmaceuticals) used in the project had been approved by the Drugs Controller General of India.
However, it was reported that many of the girls had fallen ill and seven of the girls had died, months after receiving the vaccine. In 2012, a PIL (Kalpana Mehta v. Union of India) was filed in the Supreme Court against the project alleging that clinical trials had been conducted on 24,000 tribal and marginalised girls in Gujarat and Andhra Pradesh without the subjects’ consent and without informing them of the risks associated with the HPV vaccine. The PIL referred to the 72nd Report of the Department-Related Parliamentary Standing Committee (PSC) on Health and Family Welfare titled, ‘Alleged Irregularities in the Conduct of Studies Using HPV Vaccine by PATH in India,’ which concluded that the project involved a “serious breach of medical ethics” and was an “established case of child abuse.”
Although the Parliamentary Committee did not conclude that the deaths were linked to the vaccine, the Committee was critical of the project and observed that “ICMR representatives, instead of ensuring highest levels of ethical standards in research studies, apparently acted at the behest of the PATH in promoting the interests of manufacturers of the HPV Vaccine.“
Accordingly, the petition challenged the licensing of the two vaccines used in the project and attempts to introduce them in the public sector. As of January 2023, the writ petition had been ‘dismissed for want of prosecution,’ indicating that the petitioners were no longer pursuing the case.
In December 2022, it was reported that the Ministry of Health and Family Welfare (MoHFW) and Ministry of Education had written a joint letter urging states/union territories to create awareness on cervical cancer prevention and HPV vaccine as well as issue necessary directions, among others, for organising HPV vaccination campaigns in schools.
This announcement came after the National Technical Advisory Group for Immunisation (NTAGI) recommended introducing the HPV vaccine in UIP for girls between ages 9-14 years. NTAGI is the apex technical advisory body to advise MoHFW on immunisation matters including the introduction of new vaccines.
Despite its 2022 advisory to state governments, the government put out a press release in January this year to clarify that the MoHFW is yet to decide on the roll-out of an HPV vaccination campaign in India.
While the HPV vaccine is not currently part of the UIP, the HPV vaccine is available in the Indian market. Yet, the low HPV vaccine acceptance in India may be attributable to the prevailing social stigma, namely, that vaccinating girls against HPV “will encourage sexual promiscuity.”
As HPV is an STI, “shaming and blaming beliefs” exist that being infected with HPV and cervical cancer is due to “incautious behaviour” including having multiple sexual partners.
Apart from social taboo, the cost of HPV vaccines may be prohibitive for a significant population in India. As per reports, imported HPV vaccines are available only in private hospitals and priced at INR 3500 to INR 4000 per dose, with two doses needed to complete the vaccination.
In a welcome development, ‘CERVAVAC’ India’s first indigenous HPV vaccine was launched in January last year. Jointly created by the Serum Institute of India and the Department of Biotechnology, CERVAVAC costs INR 200 to INR 400 per dose. A 2-dose or 3-dose schedule is recommended depending on the age of the individual.
Other policy measures to prevent and address cervical cancer
While a decision on an HPV vaccination campaign is awaited, the government has taken various initiatives related to cervical cancer screening and treatment.
The Operational Framework: Management of Common Cancers (released by the MoHFW in 2016) notes that cancer of the uterine cervix, breast and oral cavity are the three most commonly occurring cancers in India, and therefore, a public health priority for the country. Accordingly, the Operational Framework guides states for the management of these three common cancers in rural and urban areas.
As part of the National Health Mission, the Indian government launched the National Programme for Prevention and Control of Non-Communicable Diseases (NP-NCD) aimed at preventing and controlling major non-communicable diseases. Under NP-NCD, clinics have been established to provide services for early diagnosis, treatment, and follow-up for common non-communicable diseases at the District and Community Health Centre levels.

The Operational Framework: Management of Common Cancers (released by the MoHFW in 2016) notes that cancer of the uterine cervix, breast and oral cavity are the three most commonly occurring cancers in India, and therefore, a public health priority for the country. Accordingly, the Operational Framework guides states for the management of these three common cancers in rural and urban areas.
One of the recommendations under the Operational Framework was instituting population-based screening including for the three most common cancers. Specifically, in the context of cervical cancer, it was recommended that women between 30-65 years of age be screened once in 5 years. Population-based screening was expected to especially benefit women as well as address inequity faced by marginalised populations in accessing health care services.
The Operational Framework also recognised the need to link cancer screening programs with cancer registries across India for greater information on the ‘incidence and prevalence of cancer and related morbidities.’
Apart from screening once in 5 years, community-level awareness is emphasised. The Operational Framework stipulates that “any individual, who approaches the health facility for screening, will not be denied on any grounds.” As per July 2023 data, 4,53,46,618 individuals had been screened for cervical cancer across various states/union territories. According to 2021 WHO estimates, fewer than 1 in 10 women had been screened for cervical cancer in the last 5 years in India.
Building on the Operational Framework further, the ICMR published a Training Manual on Visual Inspection with Acetic Acid (VIA), the stipulated test for cervical cancer screening in the Operational Framework. The objective behind the Training Manual is to create a workforce competent to perform cervical cancer screening at Primary Health Centres (PHCs).
The National Cancer Grid (NCG), an initiative of the Indian government, is a network of over 200 major cancer centres, research institutes, patient groups and charitable institutions across India, covering 60 per cent of cancer care in the country. The NCG is mandated to establish uniform standards of patient care for the prevention, diagnosis, and treatment of cancer, providing specialised training and education in oncology and facilitating collaborative basic, translational and clinical research in cancer.
In 2019, the NCG released ‘Consensus Evidence Based Resource Stratified Guidelines on Secondary Prevention of Cervical, Breast and Oral Cancers.’ The Guidelines were aimed at helping states in India develop evidence-based screening, diagnosis, and management protocols for common cancers, considering that different states have different human resource capacities.

In August 2020, the World Health Assembly passed a resolution calling for cervical cancer elimination and adopting a strategy to realise this goal. Consequently, in 2020, the WHO launched the ‘Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem,’ which proposed targets that countries must meet by 2030 on the path towards cervical cancer elimination.
This strategy called for 90 per cent of girls to be fully vaccinated with the HPV vaccine by the age of 15 years, 70 per cent of women to be screened with a high-performance test by 35 years of age and again by 45 years of age, and 90 per cent of women identified with cervical disease to receive treatment (the ’90-70-90 targets’). India is one of the 194 Member States of the WHO, and therefore, is expected to honour the commitments made by the WHO.
Way forward
Cervical cancer prevention is directly related to UN Sustainable Development Goal 5 on gender equality and empowerment of women and girls. This is because a significant contributor to cervical cancer is the “lack of gender equality for women” for access to health care in many countries. Implementing prevention and control programs related to cervical cancer improves women’s health by enhancing universal access to sexual and reproductive health services.
Given the proven efficacy of vaccines in preventing cervical cancer, the Interim Budget 2024-2025 announcement is a step in the right direction for India. The government must prioritise the rollout of a nationwide HPV vaccination campaign aimed at creating awareness and debunking social myths about cervical cancer. Further, including the HPV vaccine in India’s UIP will ensure that the vaccine is accessible and available to everyone.
However, when including any HPV vaccine in the UIP, the government must do so only after studying the vaccine’s efficacy on Indian girls and women, in line with the 2022 recommendations of the Department-related PSC on Health and Family Welfare.
This will also be in line with the recent commitments made by world leaders under India’s G20 Presidency to ‘change norms, attitudes and behaviours that perpetuate gender inequality,’ and to secure women’s health and well-being.
About the author(s)
Devika is the founder of'Women & Justice', a research project that analyses how the legal justice system in India interprets women's rights and its reflection on societal attitudes towards women. She is on Twitterand LinkedIn