“Condom ke saath pleasure nahi milta,” this is what Mamta’s* partner says to her when she asks him to use protection during intercourse. Based in South Delhi’s Dakshinpuri, Mamta is a 31-year-old who has been married for 10 years, with two children aged 9 and 5. She does not want a third child. “He asks me to use contraception instead,” she says. She now uses Mala D – oral contraceptive pills. “The pills take a toll on my body – they delay my periods by over 15 days and I had even developed an infection once,” she says. Mamta’s testimony is reflective of the National Family and Health Survey 5 data on the gender gap in contraception usage in India.
The survey found that among married women age 15-49, there has been a more than ten percent increase in contraception usage, making it 66.7 percent in 2019-20. What also makes for concerning stats is how despite a significant rise in the use of condoms, female sterilization has been the most sought-after birth control measure with an adoption rate of 37.9 percent.
In an article for LiveMint, Sonal Dua, Aditi Singhal and Divya Gupta, assistant professors at O.P. Jindal Global University, analyse if this trend is because of increased female sexual autonomy or the opposite: the subjugation of women and denying them sexual and reproductive autonomy.
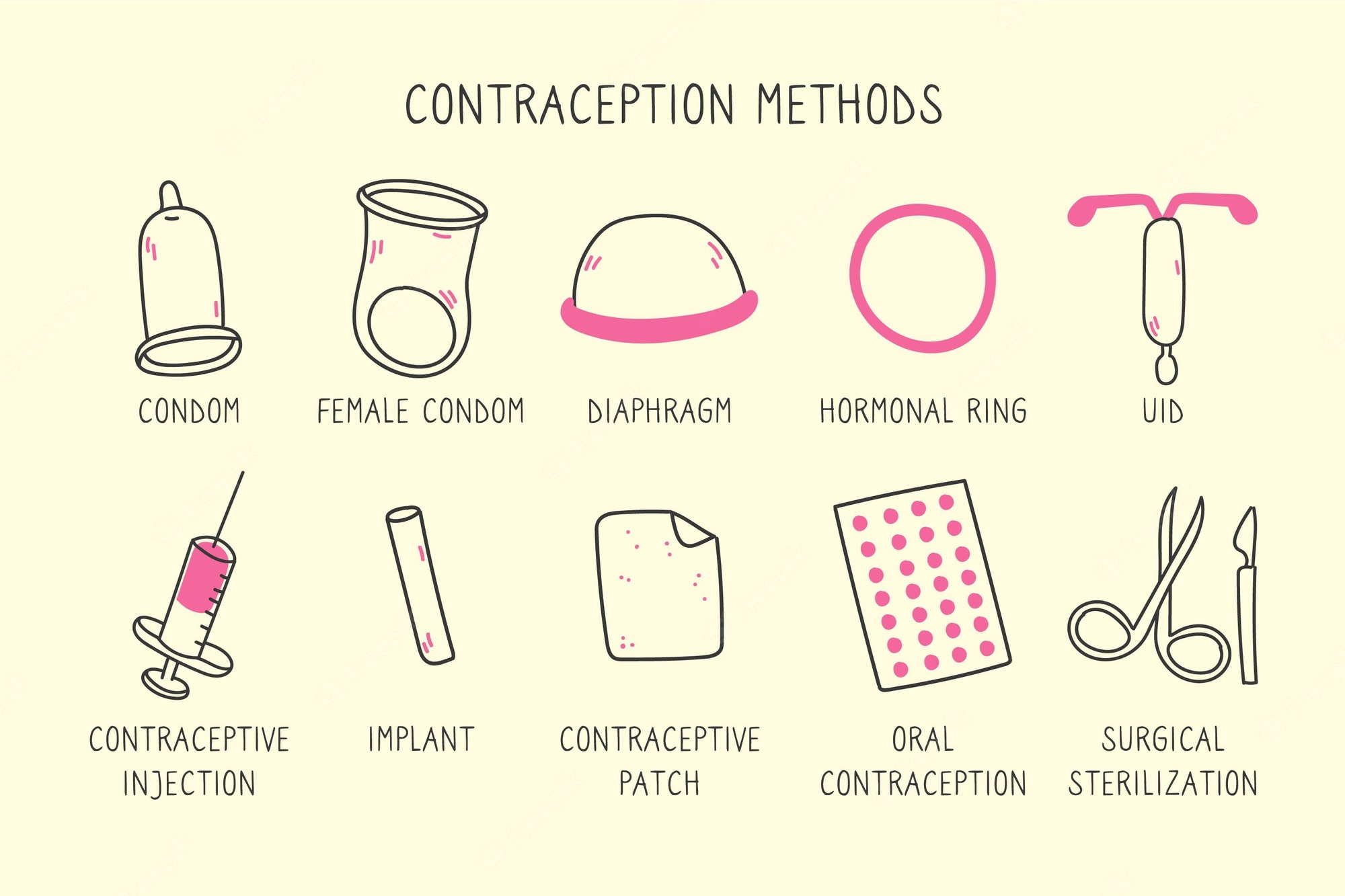
Also read: 8 Different Kinds Of Contraception To Use
Anecdotal evidence gathered from ASHAs and young mothers in Dakshinpuri suggests that female sterilisation and consumption of oral contraceptive pills such as Mala D continue to be popular forms of birth control measures, because, in many households, men refuse to use condoms or because of the popular myth in communities that vasectomy, the reversible procedure of male sterilization, adversely affects the man’s fertility.
The ASHAs gave more context to the deeply-entrenched popular misconceptions about male contraception that people continue to harbour. “When we approach the community members to talk about contraception, they often push their wives ahead to engage with us,” says Heena, an ASHA working in J Block, Dakshinpuri for about 10 years now.
How can we create an environment wherein more accountability and responsibility could be expected from men? Out of the entire range of contraceptives available, only two – condoms and vasectomy – are for men.
“Hamaare saath koi male ASHA saathi bhi nahi hai, to wo jhijhakte hai humse baat karne mei (Since we also do not have male ASHAs working with us, the men hesitate in talking to us about these issues).” Heena and Anita, another ASHA posted at J Block both observed that many men they have interacted with, directly or indirectly, think that vasectomy will affect their sexual prowess and their ability to return to work the next day.
“Not just men, their wives too, have ingrained the idea that vasectomy might adversely affect the men’s health,” says Anita. So, in addition to men pressuring their wives to undergo sterilization, many women who have undergone several abortions and multiple childbirths, voluntarily come forward instead to undergo tubectomy, she adds. Tubectomy is the female sterilisation procedure which is irreversible as opposed to vasectomy, the reversible procedure meant for cis men.
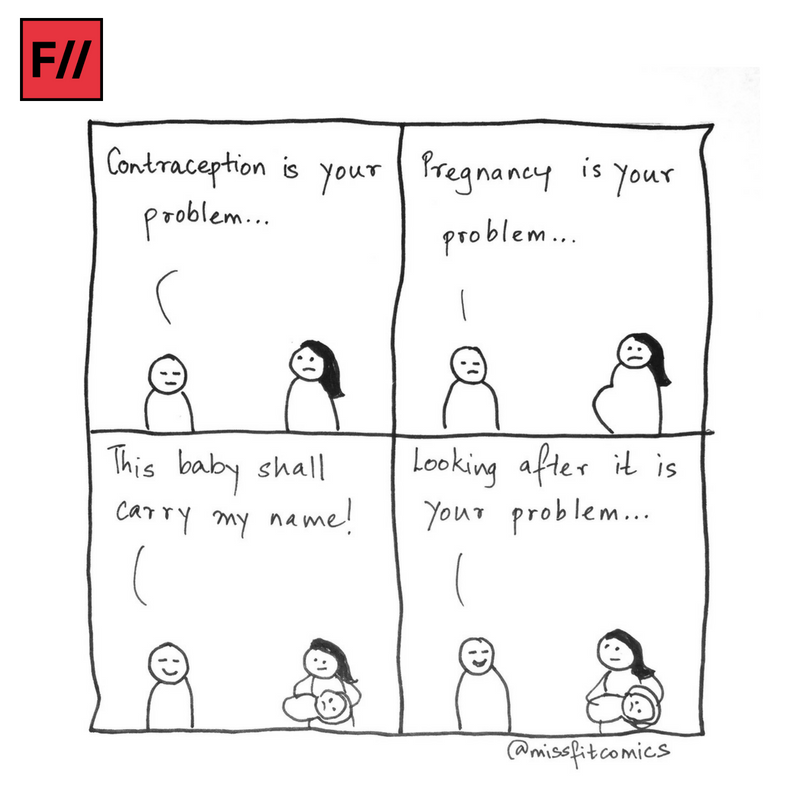
Dr Suchitra Dalvie, co-founder and coordinator at the Asia Safe Abortion Partnership, points out that the question we need to ask is: How can we create an environment wherein more accountability and responsibility could be expected from men? Out of the entire range of contraceptives available, only two – condoms and vasectomy – are for men. “And their contributions towards using those is dismal to the extent that female condoms had to be invented to reduce HIV infections. In a way, it is good that many women have access to sterilization, because that is one way of navigating the constant pressure of child-bearing,” Dr Dalvie explains.
Anita and Heena agree. “Many women come to us directly after the birth of their second or third child and say, ‘Didi, ab hume operation karna hai!’“—This often happens after multiple failed conversations at home, they say.
Engagement of men as clients, partners and service providers
As a step in the direction of bringing more men on board, Heena uses role-modelling as a technique. “I ask men who have undergone the procedure to speak to other men in the community about its benefits,” she explains. “I tell them that men can get a vasectomy done today and go back to work the next day – but hearing this from a man might help better.“
This is also a commentary on the absence of men as providers of primary healthcare dissemination. In several cases, young wives do not have the space to exercise agency to express interest in contraception and its benefits. “They often have to ask the permission of the mothers-in-law, who in turn ask their husbands,” explains Anita.
In a country where comprehensive sexuality education is yet to be an on-ground reality, young women having to discuss birth control and family planning measures with the elders in the family might seem difficult.
In a country where comprehensive sexuality education is yet to be an on-ground reality, young women having to discuss birth control and family planning measures with the elders in the family might seem difficult. This is where the engagement of male service providers to disseminate healthcare information to men becomes important. The National Health Ministry website’s description of the ASHA as someone who should be “primarily a woman …between the age of 25-45” indicates how childcare, maternal health, family planning, etc. eliminate men’s role and accountability.
On this note, an initiative by INGO Restless Development India aims to sustainably engage cis male parents in Dakshinpuri. By facilitating multiple conversations with experts, community meetings and door-to-door visits, the youth facilitators of this programme are being trained to aim in bridging the gender gap in the contraception and family planning discourse.
Also read: The Unequal Burden Of Contraception | #MyBodyMyMethod
Several studies and papers have also indicated towards policy-level interventions to bring in more male ASHAs or primary healthcare workers to address maternal and child health, sexual and reproductive health and implement family planning measures.
After all, as Dr Dalvie says, “A woman can become pregnant only once a month when she ovulates, whereas a man can get someone pregnant every time he has sex. So really speaking, cis men need to invest more or at least equally as women in the contraception discourse, in terms of accountability.”
* Some names have been made anonymous to ensure safety.
About the author(s)
Soumya is a Masters graduate in gender from Jamia Millia Islamia & has a PG Diploma in New Media from Asian College Of Journalism. She is learning to unlearn and question patriarchal structures with empathy. She has taken an interest in gardening but has over-watered and killed two plants already. This may or may not be a metaphorical reference to how she deals with life.