Posted by Renuka Motihar
The COVID-19 pandemic and strict lockdown in India have affected reproductive services such as maternal health, family planning, and abortion services adversely. While medical facilities and retail chemists were exempted from the lockdown, the curbs on movement, as well as enhanced fear of infection among patients and health providers, resulted in low availability of services. So, while the Government of India deemed RMNCAH+N (Reproductive, Maternal, Newborn, Child, Adolescent Health and Nutrition) services as essential in mid-April, access and availability continued, and continues, to be a big challenge.
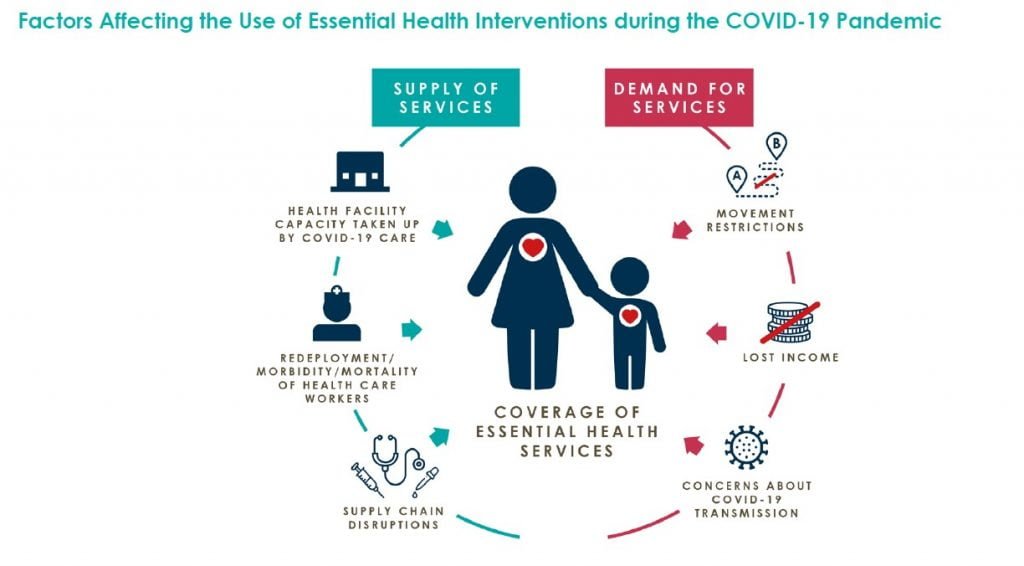
The factors affecting the use of essential health services are on both the supply and the demand sides. On the supply side, there are concerns of fear of exposure, inadequate PPE, staff being infected or under quarantine, redeployment and shortage of trained staff, overstretched health infrastructure and personnel, and lack of beds. There are newspaper reports of health facilities being overwhelmed by large numbers of COVID-19 patients needing management and treatment, especially in the hotspots. On the demand side, there is a lack of information on the status of available services, as well as increased fears and concerns of being exposed, exacerbated by the fact that RMNCH facilities are not stand alone (as they are usually available in hospitals).
This situation has led to a prevailing feeling that gains made in the country to address preventable maternal, newborn, and child mortality and morbidity in the last two decades will be reversed by COVID-19. According to estimates by health experts, millions of couples have lost access to family planning services, and there is an anticipation of an increase in unintended pregnancies, child births, and maternal deaths.
Here is a glimpse of what maternal health, family planning, and abortion services looked like during the lockdown, and what the future might hold as a result.
Maternal Health
Mathematical model estimates shared in a recent Global Financing Facility (GFF) brief indicate that large service disruptions in India have the potential to leave more than 4 million women without access to facility-based deliveries. As a result of disruptions in essential services, child mortality in India could increase by 40 percent and maternal mortality by 52 percent over the next year.
In the last few days, there have been newspaper reports of pregnant women dying as they were denied access to care. According to one such report, “A woman in the eighth month of pregnancy died in an ambulance after eight hospitals either referred her to another facility as she showed symptoms of COVID-19, or cited lack of beds.”
In the last few days, there have been newspaper reports of pregnant women dying as they were denied access to care. According to one such report, “A woman in the eighth month of pregnancy died in an ambulance after eight hospitals either referred her to another facility as she showed symptoms of COVID-19, or cited lack of beds.”
Media reports citing data from Uttar Pradesh, Bihar, West Bengal, Jharkhand, Odisha, and Chhattisgarh highlight that the number of institutional deliveries may have fallen by as much as 40 percent during the lockdown, with many women giving birth at home. That’s a significant reduction, given that a rise in institutional deliveries is believed to be one of the prime reasons India had reduced maternal and infant mortality in recent decades.
Additionally, according to Sujoy Roy from CINI and White Ribbon Alliance for Safe Motherhood in West Bengal, suffering due to COVID-19 has been exacerbated by the devastation caused by Cyclone Amphan to homes and livelihoods. There is confusion and lack of information among pregnant women and their families on where to go for health services, as hospitals are now dedicated to COVID-19.
In the midst of all this gloom, there are positive stories of facilities that have continued to provide services despite challenges and are helping women and families in need. A video report from end-May highlights the important and challenging work of doctors and nurses at the Cama Hospital in Mumbai for poor pregnant women who are reaching the hospital at the last stage during labour, with their COVID-19 status unknown. They also have a ward for COVID-19 positive mothers.
Additionally, nonprofits and hospitals are increasingly turning to technology. For example, ARMMAN, a Mumbai-based nonprofit organisation, launched a pan-India free virtual OPD system with the help of volunteer doctors. There are also anecdotes of private practitioners and hospitals giving consultations and information by phone, video, and WhatsApp, minimising contact. One other positive note, according to Manju Chhugani, a nursing educator and maternal health advocate, is that, “Caesarian Section (CS) rates have fallen and normal deliveries have gone up”. This is positive news as experts were concerned about the recent rise in CS numbers.

Family Planning Services
The lockdown has meant that access to and use of contraception has been compromised to a large extent. In line with Ministry of Health and Family Welfare, Government of India’s advisory, public facilities suspended provision of sterilisations and intra-uterine contraceptive devices (IUCDs) during the lockdown. Curbs on movement in urban areas and for ASHA workers in rural areas made access to over the counter contraceptives (OTC), condoms, oral contraceptive pills (OCPs), and emergency contraceptive pills (ECPs) difficult.
The lockdown has meant that access to and use of contraception has been compromised to a large extent. In line with Ministry of Health and Family Welfare, Government of India’s advisory, public facilities suspended provision of sterilisations and intra-uterine contraceptive devices (IUCDs) during the lockdown. Curbs on movement in urban areas and for ASHA workers in rural areas made access to over the counter contraceptives (OTC), condoms, oral contraceptive pills (OCPs), and emergency contraceptive pills (ECPs) difficult.
In an attempt to understand the impact, Foundation for Reproductive Health Services India (FRHS India) released a policy brief highlighting estimates of loss of services. Using supply side data of clinical family planning services and sales of OTC in 2018 and 2019, FRHS India has attempted to estimate the impact for three scenarios—best case, likely case, and worst case. Their findings paint a dismal picture:
- In a best case scenario, they estimate that as a result of the pandemic, 24.55 million couples would not be able to access contraceptives in 2020. In the most likely scenario (where clinical family planning services operate at full capacity by September 2020, and commercial sales of OTC contraceptives are able to resume in a phased manner by third week of May) they estimate that 63 million couples would have not been able to access contraception services during the period of the lockdown and the weeks leading up to complete normalcy, i.e., September 2020. They estimate that this loss of service will likely result in an additional 38 million unintended pregnancies, 679,864 child births, 1.45 million abortions (including 834,042 unsafe abortions), and 1,743 maternal deaths.
Also read: How Does The Pandemic Impact Adolescents?
Access to Abortion
A recent study conducted by Ipas Development Foundation (IDF) assessed the impact of COVID-19 on abortion access in India in the three months following the commencement of the lockdown (25 March 2020 to 24 June 2020). According to them, abortion access was compromised at all points of care, including public and private sector facilities and chemist outlets. The study concluded that “of the 3.9 million abortions that would have taken place in three months, access to around 1.85 million was compromised due to COVID-19 restrictions.”
The reasons include disruption in the supply chain for drugs and commodities, redeployment of facilities and staff for COVID-19 care, closure of some private facilities, lack of transport, and restricted mobility. However, the situation is expected to improve with the opening up of the lockdown. The study highlights the need for an integrated recovery plan for improving abortion services. It stresses that “many of these 1.85 million women will be coming into public and private hospitals seeking second-trimester abortions, and services should not be turning them away a second time.”
Additionally, on-ground reports from West Bengal highlight that prior to the pandemic, abortion was already shrouded in secrecy, and in these trying times with lack of access, women, in desperation, have been resorting to unsafe abortions that could lead to dire outcomes.
On the positive side, service provision organisations such as Family Planning Association of India (FPA India) and Foundation for Reproductive Health Services India (FRHS India) have continued to provide family planning and safe abortion services as far as possible, and others, such as CEHAT, have helped women access services.
Also read: How Does A Day Look Like In The Life Of A Mental Health Professional
We are realising now that COVID-19 is here to stay for longer than originally anticipated. As the pandemic continues, what can we do to ensure the availability of timely and quality maternal health, family planning, and abortion services?
—
Know more
- Read this article on how problems of access to abortion persist under lockdown, inspite of it being listed as an essential service.
- Learn more about the pros and cons of C-Sections and why their growth in India has been termed an ‘epidemic’.
Renuka Motihar is an independent consultant working on social development issues. With a background in the social sciences, Renuka works in the areas of young people’s health and development, reproductive health, and broader social, leadership, and gender related issues. Renuka has worked as a programme consultant with various international and national agencies, including UN agencies, private foundations, and nonprofits. Her focus has been on programme planning and strategy; landscape assessments and analyses; and impact assessments and programme evaluations.
This piece was first published on India Development Review (IDR) and has been re-published here with consent.
Featured Image Source: Renuka Motihar
About the author(s)
India Development Review (IDR) is India's first independent online media and knowledge platform for the development community.